potential complications
No one wants unexpected problems, complications and costs. For these reasons Dr. Paley is very conservative regarding many aspects of the limb lengthening process. Dr. Paley tries to anticipate problems and prevent complications. Many complications lead to additional surgery and therefore to additional costs. This is why experience matters, and why you should contact us today. The following is a list of some of the potential complications.
FAT EMBOLISM
In order to insert the Stryde nail in the bone the surgeon has to drill open the bone by a process called reaming the bone. Reaming leads to increased pressure in the bone (like inserting a plunger into a syringe) which causes the fat in the bone marrow to be displaced. Some of it is pushed into the circulation. When this fat gets filtered by the lungs it is called a fat embolism. Small amounts of fat are well tolerated by the lungs and lead to no symptoms.
Larger amounts can lead to shortness of breath and lower oxygenation. In the majority of cases this is treated by breathing oxygen through a nasal cannula for a few days. In more severe cases a mask with oxygen is used instead. Finally, in the very rare and most severe cases of fat embolism syndrome (FES), the patient may require transfer to the ICU including intubation and ventilator treatment.
Patients can even die from a fat embolism. To date, we have never had a patient die of FES, and only one patient required ICU treatment. To reduce the risk of Fat Embolism we use special reamers that don’t raise the intramedullary pressure as much. Dr. Paley also developed and published his technique of venting the intramedullary canal by predrilling the osteotomy site. We also adjust our rate of reaming in surgery according to the intraoperative pulse oximetry and blood pressure data. With all of these precautions our incidence of symptomatic fat embolism requiring treatment is 4%. Smoking or vaping damage the lungs and predispose patients to greater risk if a fat embolism occurs.
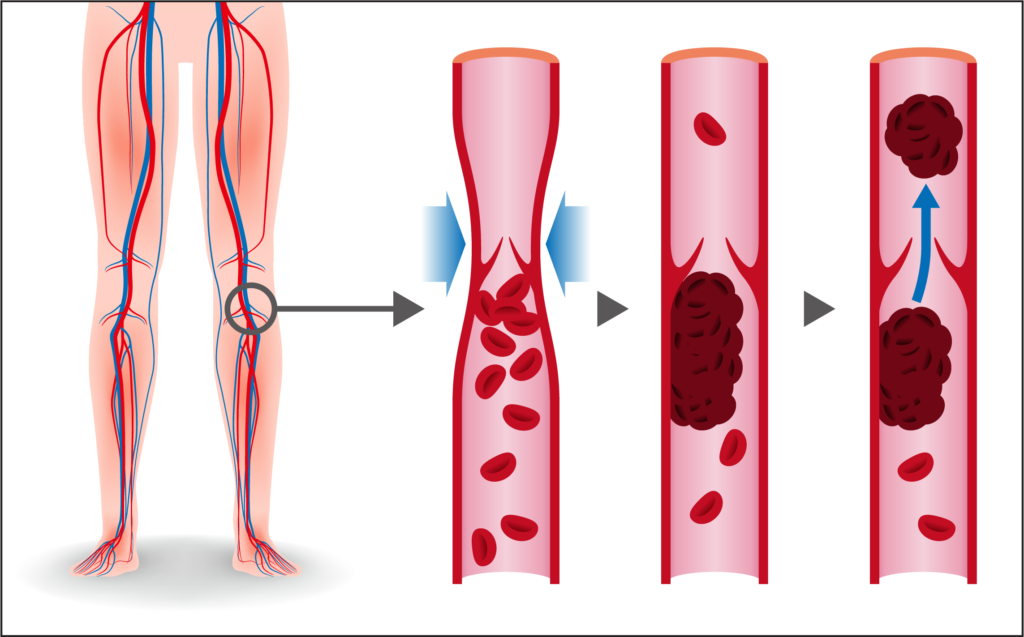
DEEP VEIN THROMBOSIS (DVT) AND PULMONARY EMBOLISM (PE)
DVT can occur after any orthopedic surgery or after any fracture. Fortunately, we have a very low rate of this complication (1%). Prevention is key. We use baby aspirin (81mg) twice a day after surgery both in the hospital and as an outpatient until the end of the distraction phase.
While we have seen very few cases of DVT, none resulted in pulmonary embolism (PE). PE occurs if the clot dislodges and wanders to the lungs. It can cause shortness of breath, chest pain, and even death. This is why we are careful to protect against this. Taking oral contraceptives and smoking increases the risk of DVT. All of our patients are placed on an anticoagulant, either aspirin or Xaralto for higher-risk patients.
PREMATURE CONSOLIDATION
In this complication, the patient’s bone heals prematurely and prevents further lengthening. Premature consolidation (PC) can occur with any lengthening method if the patient is a very rapid bone healer. The patient in these cases is able to make bone faster than the speed at which the bone is being lengthened. The only way to prevent this is to speed up the lengthening intentionally for a week or two. The Stryde nail, with its excellent rate control, allows the surgeon to do this. If premature consolidation does occur, it requires a small outpatient surgery to re-break the bone through a tiny incision. The incidence of this complication is about 1%. This is one of the few complications that can lead to additional cost to rebreak the bone. We cannot predict who is going to be too rapid a bone healer.
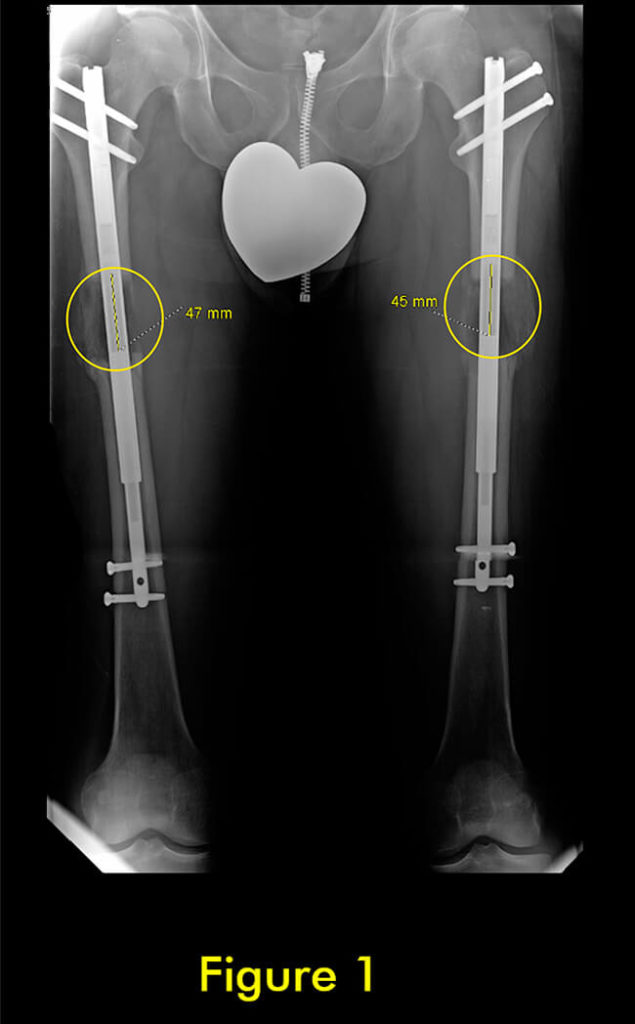
FIGURE 1:
This patient underwent femur stature lengthening at the usual 1mm per day. Seven weeks after surgery we noticed a subtle difference in the amount of lengthening (47mm right versus 45mm left).
We suspected premature consolidation based on the amount of bone visible at the lengthening site. We temporarily increased the rate of lengthening to 1.5mm per day and took new x-rays 5 days later.
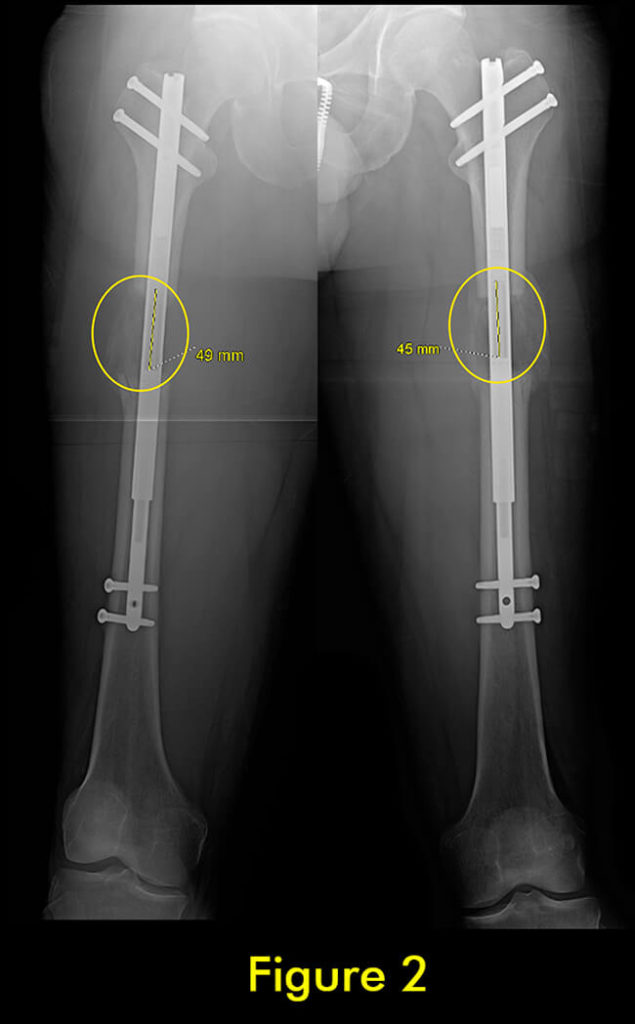
FIGURE 2:
5 days later we noted a small increase on the right (from 47 to 49mm) which was not as much as expected. On the left he did not lengthen at all. We confirmed the diagnosis of premature consolidation.
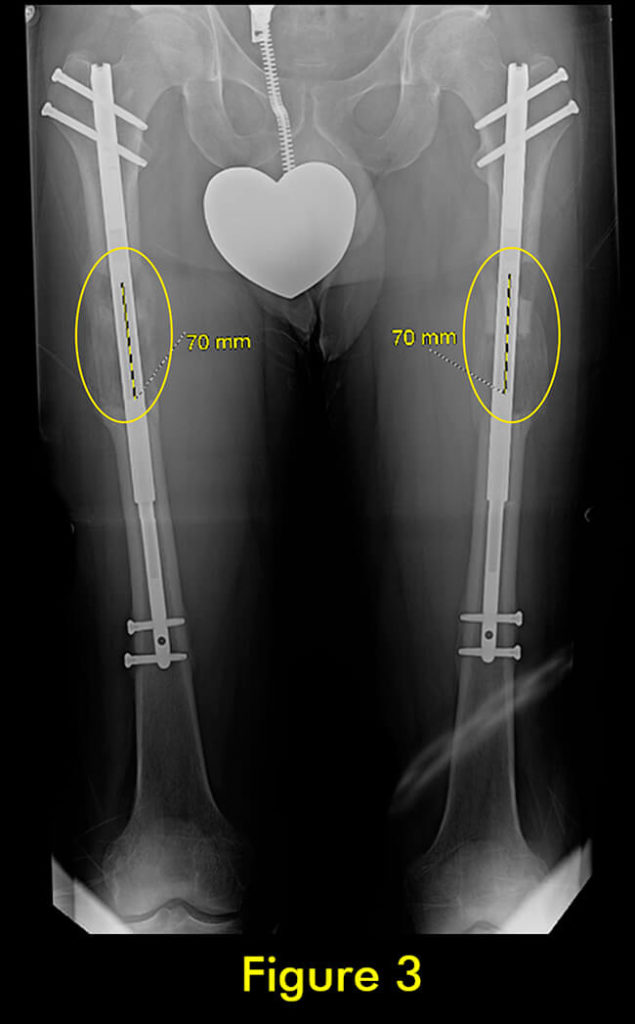
FIGURE 3:
We performed repeat osteotomies of both femurs as an out-patient procedure and finished lengthening at 70mm. FIGURE 4: Three months later he had fully consolidated.
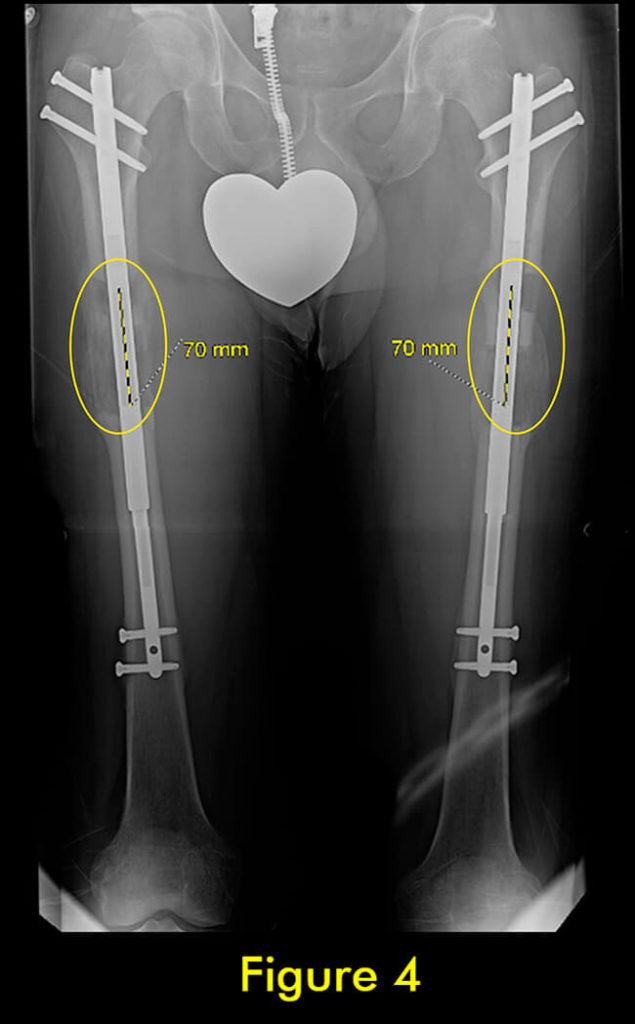
FIGURE 4:
Three months later he had fully consolidated.
DELAYED OR FAILURE OF CONSOLIDATION
Slow or failed bone healing can occur with any lengthening surgery. The best treatment is prevention. We start by identifying factors that may slow healing prior to surgery: osteoporosis, rickets, menopause, low Vitamin D level, smoking/vaping including second-hand smoke, anti-inflammatory medicine use, anti-convulsant medication use, and other medication use (e.g. acutane, biologics, steroids). We also recommend supplements to help the bone heal faster (Silical). All patients are placed on Vitamin D supplements to prevent delayed healing.
Since 2011 when we started with the Precice nail, not one patient required surgery to treat delayed or failure of consolidation. All were successfully treated by nonoperative methods including Zolidronic Acid infusion, parathyroid hormone (Forteo), Vitamin D, and other supplements and Exogen bone stimulator. If delayed healing occurs despite all of the above steps, we start using the accordion technique. Using an ERC device the bone is compressed one mm per day and distracted one mm per day. This cycle is repeated several times a day. This stimulates bone healing and avoids the need for surgery.
If surgery is necessary we know how to get the bone to heal with surgery. We got this experience when we used some of the older implantable nails that did not have rate control (e.g. ISKD). Failure of bone healing occurred not infrequently. We therefore got very proficient at using bone and bone marrow grafting to get the bone to heal. While we hope not to ever need this with the Precice or STRYDE nails if we do need this as a fall back we are very experienced on managing this complication as needed. It is critical for a surgeon to know not only how to do the surgery but also how to manage all of the potential complications.

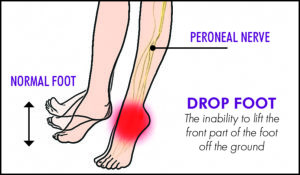
NERVE INJURY
Nerve injury can occur with any lengthening surgery but is quite uncommon if the rate of distraction does not exceed 1mm per day and if the amount of lengthening is restricted. Rate control is the most important factor to prevent nerve damage. Recognition of nerve symptoms is important.
The lengthening should be stopped or slowed in such cases. If any motor symptoms (weakness or paralysis of muscles) occur, a nerve decompression surgery should be done as soon as possible. This is a small outpatient surgery. In most cases, it is the peroneal nerve that gets into trouble. It is important that the surgeon knows how to decompress this nerve to prevent foot drop. Delay in decompression can lead to permanent foot drop. With the Stryde due to excellent rate control, nerve injury is very rare. Nerve irritation can also be treated medically using Neurontin or Lyrica.
A particular minor nerve injury is the small branch to the extensor hallucis longus muscle. This nerve is at risk from osteotomy of the fibula which we do as part of tibial lengthening. This nerve injury leads to a drop big toe which causes almost no noticeable problem. While this complication is very uncommon, it if does occur there is no treatment except to wait for the nerve to recover spontaneously which it usually does.
MUSCLE CONTRACTURES
Muscles normally get tight with lengthening. A muscle contracture occurs when a muscle gets tight enough to prevent a joint from moving through its entire range of motion. To prevent muscle contractures, physical therapy (PT) is essential.
The patient should do daily stretches of the muscles and joints at risk (e.g. knee joint and quadriceps muscles for femur lengthening and ankle joint and Achilles tendon for tibial lengthening). In addition to formal PT, the patient should do his or her own stretches at home several times per day. PT is essential to the lengthening process. It is however expensive. I will not consider doing a lengthening if a patient is not willing to do PT. This is not an option for reducing cost. The controlled rate of lengthening with the Precice makes the risk of muscle contractures and muscle spasm less. The Precice does not obviate the need for PT. Maintaining range of motion and preventing contractures during lengthening decreases the rehabilitation time to return to normal function after the lengthening is finished.
A fixed contracture of the knee or ankle can lead to disability and the need for more prolonged PT and associated expenses. If, despite additional PT, the contracture does not resolve, additional surgery to lengthen muscles, tendons, and fascia may be required. I try and anticipate this and prophylactically lengthen certain soft tissue structures to prevent contractures (e.g. iliotibial band (ITB)). If this is done at the initial surgery, the additional cost is small. If soft tissue lengthening surgery is required at a later date, the cost is much higher since one also has to pay for the hospital costs.
While there are no consequences from lengthening some muscles or tendons, such as the biceps tendon or the ITB, some tendon lengthenings can lead to permanent weakness and should be avoided. The gastro-soleus muscles with their Achilles tendon is such a case. Lengthening of this structure in an adult frequently leads to permanent weakness of push off which affects running and jumping. Some surgeons liberally lengthen this structure in association with tibial lengthening in order to obtain more length. We avoid doing this since the patient will never regain their previous ability to run and jump again. For this reason we are usually limited to 5cm of lengthening of the tibia which prevents needing to lengthen this muscle/tendon.

FIBULAR COMPLICATIONS
With tibial lengthening, the fibula has to be lengthened too. The implantable lengthening device only lengthens and fixes the tibia. The fibula has to be fixed to the tibia so that it lengthens together with it. If the fibula is not fixed or not fixed adequately, it will not lengthen as much as the tibia and will lead to severe consequences including subluxation and arthritis of the ankle and flexion contracture of the knee.
The method of fixation is critical. Many surgeons only fix the lower end of the fibula to the tibia. This can lead the fibula to prematurely consolidate and to pull down and dislocate from the tibia at its upper end. It is important to fix the fibula at both ends. Most surgeons avoid this since it is technically difficult to do.
We fix the fibula at both ends in all of our patients. With implantable lengthening, the fibula must be fixed with screws to the tibia; one screw at the upper end, and one at the lower end. The angle, level, position, diameter, and type of screw are all important. A common mistake is to put the screw in horizontally between the two bones. This is not strong enough to prevent the fibula from pulling away from the tibia at the ankle. This is very subtle and even a few millimeters of difference in length of the fibula at the ankle can lead to short term and/or long term consequences for the patient. Removing a segment of the fibula to prevent the fibula from not separating is another common method that should be avoided. It leads to a nonunion of the fibula, which can lead to a stress fracture at a later date in the tibia.
Furthermore, it usually does not prevent the fibula from pulling away from the tibia. Therefore fibular complications have nothing to do with the type of implantable lengthening device but rather with the method the surgeon chooses to fix the fibula to the tibia and the method of cutting the fibula bone. Fibular bone healing can range from premature consolidation to complete failure of union. The latter often requires no treatment as long as the tibia is solidly healed. The former requires a repeat osteotomy of the fibula.
AXIAL DEVIATION
Axial Deviation or deformity secondary to lengthening is not an uncommon problem. It can usually be prevented. Varus deformity is more likely with the use a trochanteric nail. For this reason, I prefer to use a piriformis entry nail. In proximal femur lengthenings if the osteotomy is done where the bone is tight around the nail the likelihood of varus angulation is unlikely. If a more proximal osteotomy of the femur needs to be performed, a medial blocking screw can prevent varus deviation.
Axial deviation is a more common problem in the tibia. The tibia tends to lengthen into valgus and procurvatum. To prevent this the nail should be inserted at the correct starting point, which is very high and as posterior as possible on the tibia on the lateral and centered on the knee in the frontal plane. If the nail has space between it and the lateral cortex above the osteotomy, a blocking screw should be inserted in this space. If the nail has space between it and the posterior cortex then another blocking screw is inserted there. I designed the STRYDE nail to resist axial deviation by also offering a third proximal locking screw (P2.2 only has two). If all these precautions are followed no flexion or valgus deformity develops with lengthening.
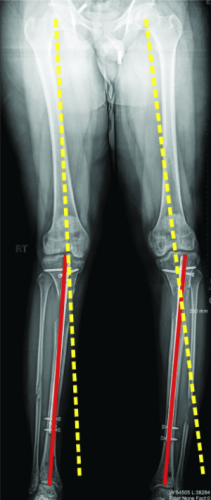
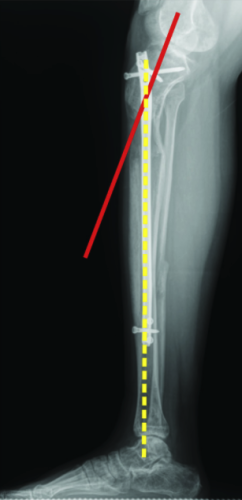
Patient who had tibia stature lengthening at an outside facility and developed complications on both sides. He developed tibia and Abu/a delayed unions, knock-kneed {valgus) on the right, bowing {varus) on the left, and f1exion {procurvatum} on both sides. We did acute corrections on both sides using a temporary external Ax ator in the operating room and placing new tibial rods. We placed retrograde rods across the Abu/a delayed unions.





